
What is a tympanic effusion?
Symptoms, diagnosis and therapy
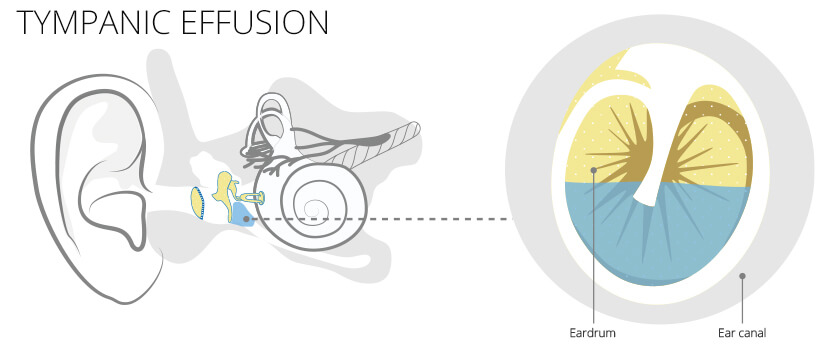
A tympanic effusion is a build-up of fluid in the middle ear. The quality of this liquid is variable. It can be serious, slimy, bloody but also purulent – depending on the cause. Tympanic effusion can be acute to chronic and has different triggers. In the following you will find out more about the symptoms, diagnosis and therapy of tympanic effusion. Effusion is a common symptom of colds, especially in children under the age of 8.
Table of Contents
- Tympanic effusion emergence
- Effusion diagnosis
- Effusion complications
- Effusion therapy
Origin and causes
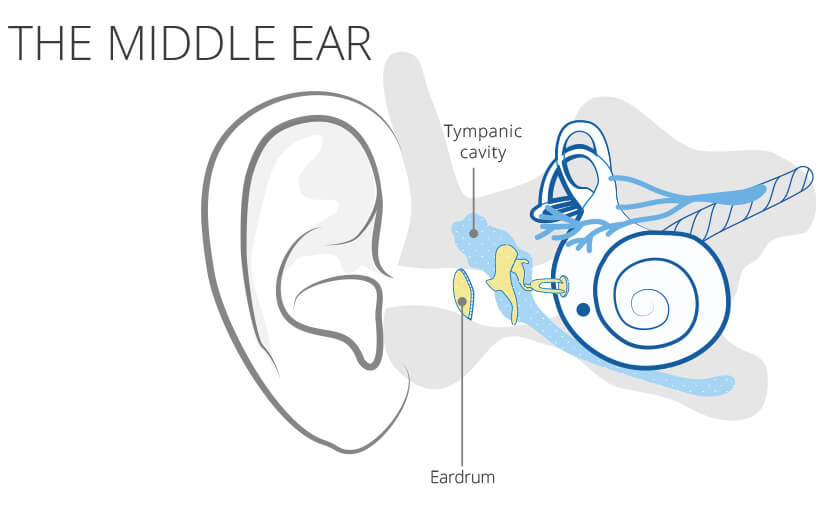
When it comes to children, the ear trumpet, the Eustachian tube, is not yet fully functional. This tube is a connection between the ear, nose and throat area and the tympanic cavity. It ensures adequate ventilation of the tympanic cavity. Since the air is absorbed in the tympanic cavity, there is always a slight negative pressure, which is balanced out with every act of swallowing. If their function is restricted, due to a cold, polyps or an enlarged pharynx, serous secretion is sucked into the space from the tissue due to the increased negative pressure. This hinders the pressure equalization.
In a chronic form that is longer than 3 months, the mucous membrane changes into columnar epithelium with goblet cells that produce mucus due to the negative pressure. Therefore, the chronic form is characterized by slimy secretion. Viruses or bacteria can turn the secretion into a purulent, painful otitis media.
Diagnosis
The doctor can look at the eardrum via an otoscopy. In the case of a tympanic effusion, he may be able to recognize a bulge (inward or outward). Fluid behind the eardrum, i.e. in the middle ear, can also be detected with an otoscopy. If the secretion is bloody, this is noticeable by a bluish shimmer. Serous secretion is amber in colour.
Tympanometry can be used to check the mobility of the eardrum and to draw conclusions about the pressure conditions. For example, if the middle ear is completely filled with fluid, the eardrum can hardly vibrate and the damping is very high.
Another examination that the doctor will perform if a tympanic effusion is suspected is a hearing test. This shows conductive hearing loss.
Complications
Hearing impairment in children can also lead to impaired speech development.
A serious complication after years is the destruction of the ossicles or a hole in the eardrum. In an emergency, these must be replaced by an implant. Inflammation threatens to spread to neighboring structures. For example, labyrinthitis, meningitis, or mastoiditis can occur. A rare but serious complication is the formation of retention pockets in the eardrum and the resulting risk of cholesteatoma. Cholesteatoma is caused by ingrowth (primary and secondary) or disintegration, during the embryonic phase, (congenital) of multilayered keratinized squamous epithelium into the middle ear. On this basis, a chronic otitis media develops, which is popularly referred to as chronic bone suppuration. This can lead to destruction of the middle ear and, in severe cases, of adjacent structures. The only recourse at this stage is surgery.
Therapy
A tympanic effusion (of the acute form) usually disappears on its own within a few days to weeks. If treatment is needed, it depends on the cause. Examples of methods for treating tympanic effusion include:
- Decongestant nasal drops to restore ventilation
- Physiotherapy: typically in the form of inhalation therapy or nasal rinsing.
- Drugs to help deal with secretions
- Antibiotics for bacterial infection
- Painkillers





